Novel Target-Specific Nanoparticles for Diagnosis and Treatment of Pancreatic Cancer
By Dr. Jill Smith
Pancreatic cancer is well known as one of the deadliest cancers, with a paltry 11% survival rate over the course of 5 years. Instances of pancreatic cancer are growing in frequency, and it is quickly becoming the second leading cause of cancer-related deaths in the United States, just behind lung cancer. Currently, the only cure for this form of cancer is surgery-but most subjects with pancreatic tumors are often not candidates for surgery because the cancer has spread at the time of diagnosis. Pancreatic cancer is not detected in the early or precancerous stage because it is not seen on routine MRI or CT scans. Therefore, most patients are only offered chemotherapy, and unfortunately, chemotherapy does not extend survival past 12 months. Early diagnosis of pancreatic cancer could improve survival of this disease.
Recent developments in novel therapies provide hope to those who are seeking a better outcome from pancreatic cancer. Advanced nanomedicines have led the charge in emerging novel therapies that could be a game changer for those afflicted with pancreatic cancer.
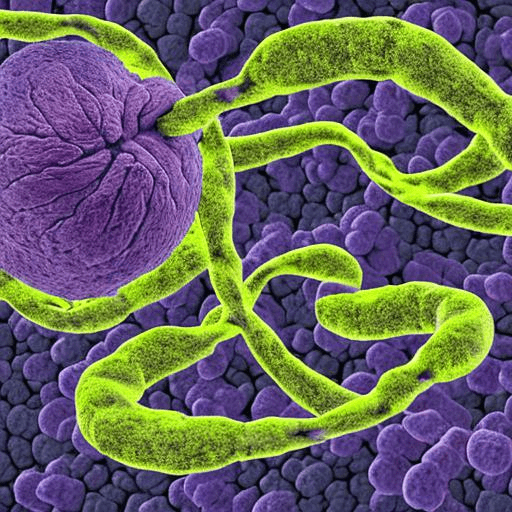
Jill P. Smith, MD, professor of medicine at Georgetown University, discovered a membrane receptor (called CCK-BR) that, while rarely found in a normal, non-cancerous pancreas, is increased in pancreatic cancer cells and microscopic precancerous lesions. In collaboration with Stephan Stern, PhD, DABT, director of R&D at the National Cancer Institute’s (NCI) Nanotechnology Characterization Laboratory, at the Frederick National Laboratory for Cancer Research. (FNLCR). Dr. Smith developed a nanoparticle-based platform that targets this receptor for treatment and early diagnosis. By attaching itself to the receptor, the nanomedicine can reveal microscopic, precancerous lesions by imaging like PET scans and deliver nucleic acid-based therapies to eradicate the lesion, improving the treatability of the condition by early detection and treatment; these nanoparticles that are utilized for both diagnosis and therapy are commonly referred to as “theranostic agents”.
A novel treatment alternative with nanoparticles gains steam
Through experiments with mice that have been genetically engineered to develop pancreatic cancer, fluorescent- and PET-labeled versions of the CCK-BR-targeted nanoparticles successfully allowed for early detection, with the nanoparticles attaching to just the CCK-BR membrane receptors rather than other tissues. Further, delivery of nucleic acid therapies to decrease pro-cancerous proteins, such as gastrin and mutant Kras, were found to halt cancer progression and treat established cancers. Researchers were also able to confirm that the nanoparticles were found only in the pancreas and not in other areas of the body, decreasing the potential for off-target toxicity.
Following the promising results of these studies performed by the team, Georgetown University worked with the National Institutes of Health (NIH), which funds FNLCR, to file patent applications on this novel nanoparticle technology. The FNLCR is a government-owned, contractor-operated national enterprise that supports the NCI, part of the NIH. Currently, there are issued patents and several pending patent applications directed to this technology that are jointly owned by Georgetown University and the NIH, with Drs. Smith and Stern as named inventors. Though it may seem like nanomedicine breakthroughs for cancer treatment are in their relative infancy, the benefits of nanotechnology are well-known within the oncology community.
The first hint at the power of nanotechnology in cancer treatment came in 1995. That year, the FDA approved the use of a liposome to deliver a more heart-friendly form of the chemotherapy drug doxorubicin. Many other therapies utilizing nanotechnology are in various stages of testing or have already gained approval for use in treatment of cancers.
Nanotechnology as a whole has become very popular within the pharmaceutical industry due to its myriad of benefits, including drug delivery, vaccines (including the current COVID-19 vaccines), and immunotherapy. Nanotechnology, and nanomedicine in particular, continues to be studied, tested, and meet approval for a host of uses.
A brighter future for cancer patients
This advanced nanoparticle technology developed by the Georgetown and FNL research team could improve the prognosis for pancreatic cancer patients. Where pancreatic cancer was once, essentially, a terminal diagnosis, earlier detection and treatment could improve overall outcomes. When pancreatic cancer can be detected at the localized stage, the 5-year survival rate increases to 42%.
Pancreatic cancer is a frightening prospect for over 64,000 people in the US annually. With further study and development, this novel nanoparticle theranostic agent could detect pancreatic cancer at its most treatable stage, improving prospects for patients whose futures were, before, uncertain.
About The Author
Dr. Jill P. Smith is a Clinician Scientist and Professor of Medicine at Georgetown University and a member of Georgetown’s Lombardi Comprehensive Cancer Center. Her passion has always been bench-to-bedside or translational research. She was the first female president of the American Pancreatic Association. She was recruited to Georgetown University from the National Institutes of Health, to establish a translational research program in GI cancer. Her basic science bench research for over 2 decades has focused on G-protein coupled receptors, in particular cholecystokinin receptors. Her laboratory discovered that CCK receptors are over-expressed in human pancreatic cancer for which she received an international science award from the European Pancreas Club. Her research focuses on pancreatic cancer and hepatocellular carcinoma in understanding the mechanisms involved with carcinogenesis and developing novel strategies for therapy or cancer prevention.
