Medical Coding & HIM Industry Faces Mounting Challenges, According to Black Book’s Latest Poll Ahead of AHIMA 2024 Conference

Eight Major Industry Controversies Set to Dominate Discussions Among AHIMA Members and Industry Experts
SALT LAKE CITY, UT / ACCESSWIRE / October 18, 2024 / Ahead of the highly anticipated annual AHIMA Conference, Black Book Research has released its latest survey of health information management (HIM) professionals, revealing critical challenges confronting the medical coding industry in Q3 2024. The report spotlights growing controversies surrounding regulatory changes, evolving coding practices, and pressing ethical concerns, bringing several key issues to the forefront.
Fraud and Upcoding Surface as Key Concerns for 2025:
90% of respondents identified “upcoding” – the practice of assigning higher-level codes than justified to increase reimbursements – as a major ethical dilemma for staff coders. An employee or staff member who is ordered to perform illegal coding duties can be referred to as a scapegoat, coerced employee, or complicit staff. In legal terms, they might be considered an involuntary accomplice if they are coerced, if they are set up to take the blame for illegal activities. This practice not only drives up healthcare costs but also exposes providers to significant penalties under Medicare and Medicaid regulations. Alarmingly, 18% of respondents reported facing pressure from their employer to engage in what they described as fraudulent coding for provider financial gain. Such practices have contributed to rising healthcare costs and an increase in legal actions, including fines and criminal charges. Looking ahead, 99% of respondents anticipate a significant rise in whistleblower cases under the False Claims Act over the next decade, signaling a heightened focus on compliance and legal accountability within the coding industry.
ICD-11 Transition Concerns:
As the industry prepares to transition to the more complex ICD-11 system, 80% of respondents expressed anxiety over the required training and potential for increased coding errors. The impending shift has prompted only 11% of provider organizations to ramp up preparations, though 87% are concerned about readiness.
Challenges with Value-Based Care Coding:
The industry’s ongoing shift towards value-based care-where providers are reimbursed based on patient outcomes – has raised questions for 64% of respondents regarding the adaptability of current coding practices. Proper documentation is crucial, but aligning systems with this evolving model remains a challenge for 29% of surveyed providers.
Risk Score Manipulation in Value-Based Care:
7% of respondents acknowledged accusations of manipulating risk scores to enhance reimbursements under value-based care programs. This practice continues to fuel concerns about the integrity of coding processes by 48% of respondents.
Coding Audits Spark Discrepancy Debates:
85% of healthcare providers argue that discrepancies identified during coding audits, often leading to denied claims or repayment demands, stem from the complexity of the current system, raising concerns about the fairness of audits.
Bundling vs. Unbundling Coding Controversy:
Over half (55%) of respondents believe bundling services into a single code underestimates the true scope of care provided, while unbundling, aimed at maximizing reimbursements, risks accusations of fraudulent billing.
Social Determinants of Health (SDOH) Coding Raises Ethical Questions:
Coding for social determinants of health – factors such as housing and education – has sparked debate, with 69% of respondents citing concerns that this could unintentionally reinforce biases in healthcare systems or affect coverage decisions.
AI in Medical Coding – A Double-Edged Sword:
The rise of artificial intelligence (AI) in coding has divided opinions. While AI and machine learning are being used to automate processes, 94% of professionals voiced concerns about the accuracy and nuance of AI-generated codes, and 97% believe critical human oversight may be lost. Additionally, 77% expressed concerns over AI’s potential to perpetuate biases in healthcare billing and access.
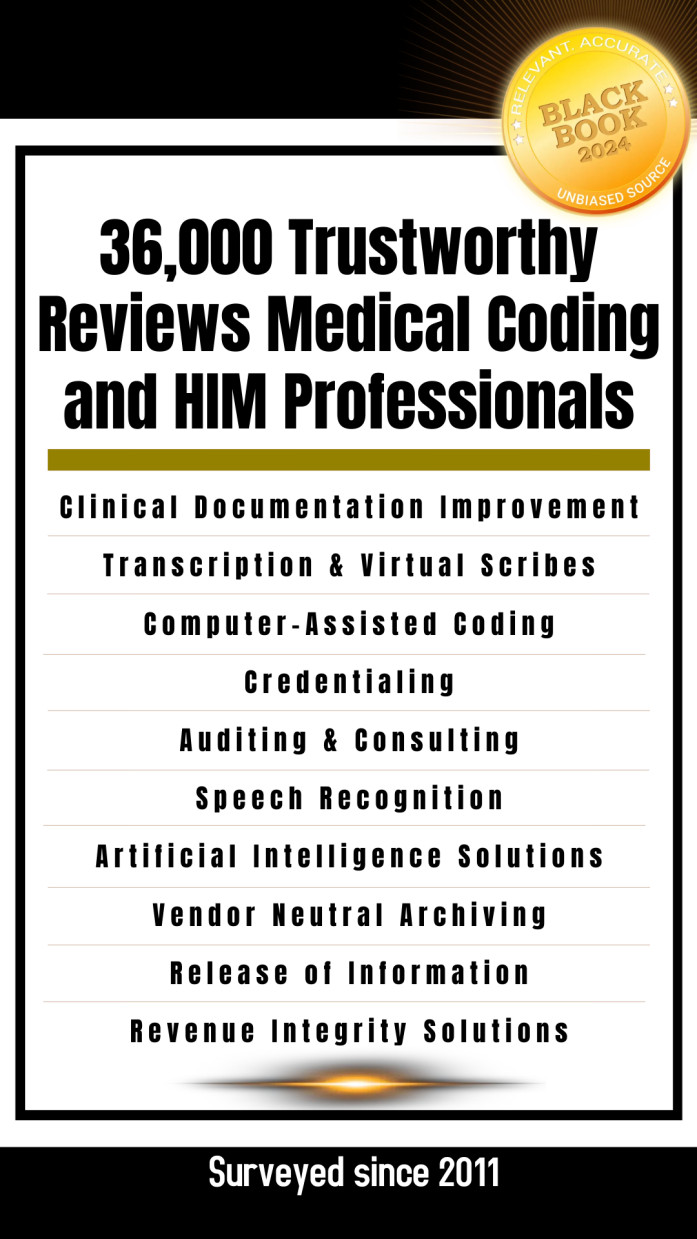
As the AHIMA Conference, scheduled for October 27-29 in Salt Lake City, approaches, these findings will likely fuel discussions around the future of medical coding, regulatory reform, and the ethical dilemmas that HIM professionals face. Black Book will be announcing the top client experience ratings for the vendors of coding, health information management, medical records and clinical documentation solutions, as well as coding and HIM outsourcing suppliers and niche HIM consultants prior to the conference at https://blackbookmarketresearch.com/coding-health-information-management
About Black Book™:
Black Book™ is a leading healthcare research and consulting firm, renowned for its expansive data lake that aggregates insights from over 2,500,000 healthcare users and professionals. This unparalleled resource enables deep analysis of industry trends, vendor performance, and client satisfaction. Since 2011, Black Book has published independent healthcare IT satisfaction and client experience rankings, ensuring transparency and objectivity by reporting results to the public and media before vendors are notified. Black Book’s founder, management, and staff hold no financial interest in the vendors evaluated, and the organization does not charge fees for participation, reviews, or consultations. 4,081 responses were recorded in this crowdsourced survey between January 31 and October 6, 2024. More information is available at blackbookmarketresearch.com.
Contact Information
Press Office
research@blackbookmarketresearch.com
8008637590
SOURCE: Black Book Research
View the original press release on newswire.com.
